Over the past few decades, Rwanda has made significant strides in tackling HIV/AIDS, but challenges remain. The country has been praised for its comprehensive response to the epidemic, including public health campaigns, access to treatment, and community support systems. However, the disease still affects thousands of individuals, and the fight against HIV/AIDS in Rwanda is far from over.
This article highlights the current situation, provides insights into the impact on local communities, and shares personal testimonies of resilience.
Current Situation:
Rwanda has made notable progress in reducing the impact of HIV/AIDS, with a decrease in both new infections and AIDS-related deaths. According to the latest data from the Rwanda Biomedical Centre (RBC), the national HIV prevalence is estimated at 3.0% for adults aged 15-49. This figure reflects an overall decline in new HIV infections, thanks in part to aggressive prevention efforts such as condom distribution, education campaigns, and testing.
As of 2023, approximately 250,000 people are living with HIV in Rwanda. The country’s efforts to ensure universal access to antiretroviral therapy (ART) have been largely successful. Roughly 90% of those diagnosed with HIV are on treatment, helping to suppress the virus and reduce transmission. Rwanda has also made remarkable progress in preventing mother-to-child transmission, with nearly 99% of pregnant women living with HIV receiving antiretroviral treatment to protect their children.
Despite these achievements, challenges remain. Stigma continues to surround HIV, preventing some people from seeking testing or treatment. The pandemic’s social and economic impact has also increased vulnerability, especially among key populations such as sex workers, men who have sex with men (MSM), and young people.
Testimonies:
Marie Claire’s Story:
Marie Claire, a 34-year-old woman from Kigali, was diagnosed with HIV five years ago. She was initially overwhelmed by the stigma that came with her diagnosis, but through counseling and support from local health services, she learned to live positively. “I was scared to tell my family and friends, but I realized that my life didn’t have to end because of HIV,” she shares. “Now, I am healthy, on ART, and I’m part of a support group that helps others living with HIV.”
Marie Claire’s testimony highlights the importance of access to treatment and mental health support. Rwanda’s community-based support groups have played a key role in helping individuals cope with the emotional challenges that come with living with HIV.
Jean Paul’s Struggle:
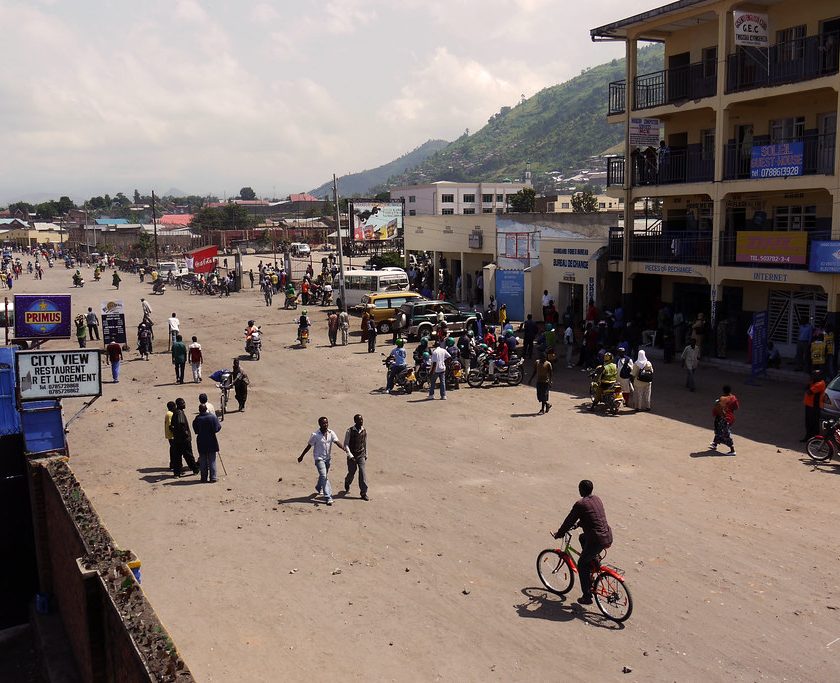
Jean Paul, a 42-year-old man from Rubavu, initially avoided getting tested for HIV due to fear of the results. After engaging in high-risk behaviors, Jean Paul decided to go for testing, and it came back positive. “When I found out, I felt like my world had collapsed,” he admits. “But I now understand that HIV is not a death sentence. I am living a normal life because I take my medicine regularly and keep a positive attitude.”
Jean Paul’s journey reflects the importance of HIV awareness and the role of testing in the early detection of the virus. Public health campaigns in Rwanda have focused on making HIV testing more accessible and reducing the fear that often surrounds it.
Isaac and the Prevention of Mother-to-Child Transmission (PMTCT):
Isaac is a father of two living in the Northern Province of Rwanda. His wife, Catherine, tested positive for HIV during her pregnancy. Through the PMTCT program, Catherine was able to receive the necessary treatment during pregnancy and childbirth, and both children were born HIV-free. “It’s been a journey for us, but I am so grateful that we were supported by the health system,” Isaac says.
Rwanda’s strong focus on PMTCT programs has ensured that children born to HIV-positive mothers have an overwhelmingly high chance of being born HIV-negative, a model that has been replicated in other parts of Africa.
Key Challenges:
Stigma and Discrimination
Despite significant progress in awareness campaigns, HIV-related stigma remains prevalent in some areas. Many people living with HIV still face discrimination in their communities, workplaces, and even in healthcare settings. This social stigma discourages many from getting tested and seeking treatment.
Vulnerable Populations
Young people, sex workers, MSM, and people in conflict zones are at heightened risk of HIV. While Rwanda’s national HIV prevention programs target the general population, these groups often face specific challenges that need to be addressed with tailored interventions.
Gender Inequality
Women, especially those in rural areas, face greater risks of contracting HIV due to gender-based violence, limited access to education, and economic dependency on their partners. Addressing these underlying factors is crucial in reducing the rate of new infections among women.
Data & Statistics:
- HIV Prevalence: 3.0% of the adult population (15-49 years old) is living with HIV.
- HIV Testing: In 2023, over 85% of the population had been tested for HIV at least once, with significant improvements in the accessibility of testing in rural areas.
- Treatment Coverage: Over 90% of those diagnosed with HIV are receiving ART.
- Mother-to-Child Transmission: 99% of pregnant women with HIV receive ART to prevent transmission to their children, resulting in low rates of new pediatric HIV cases.
Government and NGO Support:
The Rwandan government, in partnership with international organizations like UNAIDS and the Global Fund, has heavily invested in the fight against HIV. National programs focus on prevention, education, and improving access to healthcare services. NGOs such as Partners In Health and Médecins Sans Frontières (MSF) have also played critical roles in supporting vulnerable communities.
Moreover, the government has introduced national policies aiming to provide comprehensive care for people living with HIV, which include free HIV treatment, regular viral load monitoring, and a robust referral system for specialized care.
Rwanda is on the path toward ending the AIDS epidemic by 2030, with ambitious goals set under the national HIV/AIDS strategic plan. Continued investment in health infrastructure, increased awareness, and efforts to tackle stigma are essential for achieving these targets.
With effective treatment and prevention programs, and the resilience of the Rwandan people, there is hope that the country will continue to make progress in its fight against HIV/AIDS.
While HIV remains a significant public health challenge in Rwanda, the country’s proactive response offers valuable lessons in the fight against the epidemic. From improving access to treatment to breaking down stigma and supporting vulnerable populations, Rwanda’s efforts reflect a holistic approach to addressing HIV/AIDS. Personal stories of survival, like those of Marie Claire, Jean Paul, and Isaac, serve as powerful reminders of the importance of community, treatment, and hope.
BY KAYITESI Ange